Showing posts with label food addiction. Show all posts
Showing posts with label food addiction. Show all posts
Sunday, 5 August 2012
Weight Loss Redux
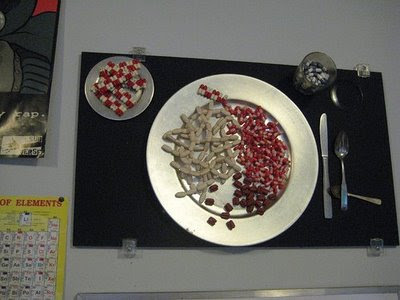
Why diet pills are problematic.
"Physicians who treat obesity hailed the Food and Drug Administration's recent approval of two new diet drugs—the first in 13 years—as a new era in weight-loss management."
--Wall Street Journal, July 30, 2012
(The following post was originally published on September 20, 2011)
It took many years to bring depression and its treatment into the rational light of day. Addiction in the mid-1990s was in the process of undergoing a similar medical transformation. Even so, scientists were wary of pronouncing that overeating was in some cases a treatable chemical disorder.
Obesity, in any form other than pituitary cases, was not typically considered a medical disorder at all. In a 1998 interview with MIT’s student newspaper, The Tech, neurology professor Richard Wurtman recalled that ten years earlier, the major drug companies had shown little interest in a drug treatment for obesity: “They thought that if you were obese, it was your fault.” It was the same view that had prevailed concerning depression, alcoholism, and other drug addictions. Bulimia and carbohydrate craving were no different: a simple failure of will was once thought to explain them all. But everything changed when the serotonin-boosting diet pill called Redux (dexfenfluramine) won full FDA approval in 1996. Redux was the first drug ever approved in the U.S. for the long-term treatment of obesity.
In truth, Ely Lilly and Company did move forward with earlier efforts to win approval of high-dose Prozac for weight loss. That petition had been languishing in the FDA pipeline for years under the trade name Lovan. Back in the late 1980s, when Eli Lilly scientists were investigating rats that consumed fewer calories on fluoxetine, the company called upon Dr. Richard Wurtman, the MIT brain scientist who specialized in the connection between serotonin levels and carbohydrate intake. Scientists at Lilly had become increasingly concerned that the weight loss from Prozac was short-lived, and the mechanism of action remained maddeningly imprecise. For more than a decade, Eli Lilly had pursued Prozac along three separate but related lines of development: depression, weight control, and alcoholism. If you took it for depression, and it worked, you might also lose a few pounds, and drink less. If you took it for bulimia or weight loss, you might also feel better emotionally, and drink less. When the FDA made encouraging noises about Prozac as a new front-line treatment for bulimia in 1994, Eli Lilly followed that indication to market, and again chose not to follow up on weight loss or alcoholism.
Eli Lilly was no longer interested, but Richard and Judith Wurtman were undeterred. As it happened, the couple had already patented a serotonin-active drug of their own—dexfenfluramine—which French laboratories had been testing as a weight loss pill. The Wurtmans went public with a new company, Interneuron Pharmaceuticals, and filed with the FDA to market their weight-loss remedy. The Wurtmans became instant millionaires on paper.
“Diet pills” had always had a somewhat unsavory reputation. Typically, they were amphetamines, or the near-beer equivalent, ephedrine—and neither compound was anything like a healthy long-term answer to chronic overeating. The serotonin-active drugs were a new class of medications altogether. Dexfenfluramine wasn’t addictive, any more than Prozac was addictive. Moreover, fenfluramine was specifically intended for use by people suffering from carbohydrate-craving obesity. But would doctors be able to resist the demands of other patients who just wanted to trim off a few pounds?
Initially, the Wurtmans licensed the serotonin-active weight loss drug to several marketers in Europe, where it met with initial success. After a few small-scale studies, Rochester University in New York published a report showing that the weight loss effect was enhanced when fenfluramine was combined with a drug called phentermine. The resulting combination was widely known as “phen-fen.” As with Prozac, dexfenfluramine was tested as an anti-obesity medication at dosages several times higher than the amount typically prescribed for depression.
Early red flags were raised when Johns Hopkins researchers reported some cases of neurological toxicity in monkeys on dexfenfluramine, but MIT, which shared patent rights with the Wurtmans, was understandably enthusiastic when Redux, as dexfenfluramine became known, won full FDA approval in 1996.
And for many people, Redux worked. In the first six months after its approval, physicians wrote at least two million prescriptions for Redux. The phen-fen combination swept the weight loss industry. Estimates of total users of phen-fen ran as high as six million in the U.S. alone. Doctors and weight loss clinics sometimes prescribed Redux, sometimes the phen-fen combination. Initial earnings estimates were running as high as $600 million a year for the Redux portion of phen-fen, netting MIT between one and five per cent of the royalties.
The euphoria didn’t last long. By the time Redux made the cover of Time, researchers were already rumbling about continued reports of high toxicity and hypertension in rat studies. In addition, the serotonin surge associated with the use of dexfenfluramine caused concerns about pulmonary hypertension. In August of 1997, doctors at the Mayo Clinic in Minnesota reported serious heart valve abnormalities in 24 women taking the phen-fen combination.
A month later, at the FDA’s request, phen-fen and Redux were permanently pulled off the market. In 2002, American Home Products settled a class action suit on behalf of almost 300,000 phen-fen users for $3.75 billion. As class action suits go, this put it right between the $2.4 billion Dalkon Shield settlement and the $4.5 billion breast implant accords.
What went wrong? Researchers now believe that the two drugs, which were never offered for sale as a single pill, should never have been combined in the first place. Somehow the fact that the phen part of the combination allegedly acted as an MAO inhibitor, and hence should not have been combined with yet another serotonin-enhancing medication, escaped notice. The combination of the two drugs apparently raised blood plasma levels of serotonin to abnormal levels. Too much serotonin in the bloodstream can damage blood vessels in the heart and lungs. Other suspected MAO inhibitors, like St. John’s Wort, or the Chinese herbal remedy ma huang, would not have combined well with Redux or phen-fen, either. Referring to the casual use of Ecstasy, Dr. Rick Doblin drew a parallel with phen-fen in the autumn 1995 issue of the Multidisciplinary Association for Psychedelic Studies (MAPS):
This use of MDMA, though not conducted in the context of a scientifically controlled experiment, does provide an opportunity for a very large epidemiological study. Similarly, over fifty million people have tried a prescription drug called fenfluramine, a diet aid prescribed for daily use for months or years at a time that causes the same kind of neurotoxicity in animals as does MDMA.
The phen-fen disaster highlighted the need to investigate drug synergies thoroughly before combining them as a pharmacotherapy. The phen-fen heart and lung damage may have been related to a potentially toxic condition known as “serotonin syndrome.”
And the Wurtmans? Ironically, Richard and Judith Wurtman had patented the use of Prozac for severe PMS years earlier, and ultimately sublicensed the rights back to Eli Lilly for several million dollars. Eli Lilly disguised the fact that their PMS drug was a case of old wine in new bottles. As Wellbutrin had become Zyban, so Prozac metamorphosed into Serafem, when prescribed for premenstrual syndrome.
Photo Credit: http://www.drugnet.net/
Wednesday, 13 January 2010
The Addiction Inbox Top Ten
What are readers of Addiction Inbox interested in? Although scarcely scientific, a look at the most-viewed posts here over the past couple of years is indicative of general interest—or at least indicative of the general drift of Google searches on topics related to addiction and drugs.
Ranked by overall page views, from most to least, here are the ten most-visited blog posts on Addiction Inbox:
The most popular post on Addicton Inbox by a considerable margin. With almost 700 reader comments, this post has evolved into a message board for people having problems related to marijuana dependence and withdrawal. Very interesting first-person stuff attached to a rather straightforward post. Continues to grow like Topsy.
A continuation of the discussion of marijuana withdrawal, or, as the director of the National Institute on Drug Abuse (NIDA) Nora Volkow calls it, “cannabis withdrawal syndrome.” 100 reader comments thus far.
Sometimes you just gotta get back to basics. Inquiring readers want to know.
A lively debate on the new, smokeless nicotine delivery system. Electronic cigarettes use batteries to convert liquid nicotine into a heated mist that is absorbed by the lungs. The latest in harm reduction strategies, or starter kits for youngsters?
Another good response to a medical post about a drug for seizure disorders and migraines that shows promise as an anti-craving drug for alcoholism. People are getting more accustomed to hearing about medications for addiction.
Not a big surprise.
Another comment-heavy post concerning a controversial study of withdrawal effects from smoking cigarettes and pot.
Something of a merger here between two consistently popular topics--cannabis and brain science. After the Sanskrit “ananda,” meaning bliss.
Readers seem to take seriously the notion that certain forms of overeating are substance addictions. This post focused on sugar's drug-like effect on the nucleus accumbens, a dopamine-rich brain structure in the limbic system.
10. Coffee Addiction
Increased tolerance, craving, and verifiable withdrawal symptoms--the primary determinants of addiction--are easily demonstrated in victims of caffeinism.
Tuesday, 12 May 2009
Bulimia: What To Look For [Guest Post]

Signs and symptoms of a dangerous disorder.
[Today’s guest post was contributed by Heidi Taylor. I include it here as part of a continuing series of guest posts having to do with the so-called “lifestyle addictions,” such as perceived addictions to gambling, sex, video games, or shopping—areas in which I can claim no special expertise, and diagnoses which remain controversial among addiction researchers. However, I do strongly believe that the case has been made for the addictive nature of certain eating disorders—bulimia and carbohydrate-craving obesity in particular—in which the ingested substance is food, not “drugs” as we commonly think of them. Eating is one of the most obvious ways in which we alter the neurochemistry of our brains every day. As for treatment, serotonin abnormalities are believed to be the culprit. Many bulimics improve on SSRI antidepressants.]
--Dirk Hanson
Detecting Bulimia in a Loved One
It’s not a disease that’s visible at first or even second sight, but even so, it is one that’s largely ignored and left untreated more because most people are not even aware of its existence. But bulimia, or to be exact, bulimia nervosa is an eating disorder that could end up having physical, psychological and sociological consequences that are hard to digest. Bulimics tend to eat more than they should – in fact, they gorge on food – and then force themselves to throw up using emetics, visit the toilet with laxatives, or go without food for the next day or so. In short, they compensate for their over-eating in ways that are neither healthy nor advisable.
While it may not seem like a dangerous disorder, bulimia can have devastating consequences if left unchecked – people affected are prone to suffer from an inflamed throat and neck glands, a torn esophagus, decaying and unhealthy teeth, acid reflux disorder, ruptured intestines, irritable bowels, dehydration and malfunctioning kidneys. Besides these physical symptoms, they’re also going to be obsessed with their weight, suffer from depression and anxiety, and face other mental and social problems. So if you suspect a loved one may be bulimic, here are a few symptoms that will help you detect the disorder and get them professional help as soon as possible:
• Eating more than the normal amount possible in a single meal or over the course of a few meals.
• Frequent visits to the toilet after a meal.
• A washed out and drained look that happens because they’re dehydrated and their body is low in minerals from all the purging and use of laxatives.
• Mood swings that seem to come on for no apparent reason.
• Sores in the mouth and/or on their fingers (because they may be sticking it in their throats to induce vomiting).
• Inflamed throats and bad teeth.
• Bouts of depression or uncalled for anxiety attacks.
• Exercising for a long time, at odd hours of the day and being obsessed with the way they look.
• It’s the women and the teenagers who are more susceptible to this disorder because of their obsession with their weight and the way they look. So if you have a daughter or a close female friend or relative who acts in a way that points suspicion to bulimia, talk to them and get them much-needed medical intervention before the situation worsens.
Even if you just suspect bulimia and are not really sure, you’d do well to talk to the person concerned and get them to see a doctor who can help. Remember, it may sound like a minor thing, but bulimia is a very serious disorder.
--------
This post was contributed by Heidi Taylor, who writes about the Masters in Healthcare. She welcomes your feedback at HeidiLTaylor006 at gmail.com
Graphics Credit: Graham Menzies Foundation
Friday, 24 April 2009
How Junk Food Works

Ex-FDA chief offers clues to food addiction.
It is a perplexingly common experience: You open a bag of cookies, intending to have one or two. An hour later, the bag is empty, and your self-loathing is at its peak.
But compulsive overeating is not a character flaw, according to David Kessler, former head of the Food and Drug Administration. It is, rather, a “biological challenge.”
Readers may remember Kessler from his anti-cigarette and food product labeling crusades during the Clinton administration. In his forthcoming book, The End of Overeating: Taking Control of the Insatiable American Appetite, Kessler notes that while food took over his brain, the foods in question were not carrots, apples and green leafy vegetables. “Conditioned overeating,” as Kessler dubs it, is driven by a biological drive to eat high-fat, high-sugar foods even when we are not hungry. Moreover, such foods are cheaper than more healthy alternatives.
What Kessler describes in his book is a system of reward-driven eating abetted by a food industry fully aware of the biological attraction exerted by salt, fat, and sugar. Kessler himself is no stranger to this attraction. “I have suits in every size,” Kessler writes, according to a report by Lauren Neergaard for AP. “Once you know what’s driving your behavior, you can put steps in place.”
Kessler has also served as dean of the medical schools at Yale and the University of California at San Francisco. On the book’s Amazon site, Michael Pollan, author of In Defense of Food, calls Kessler’s book “a fascinating account of the science of human appetite, as well as its exploitation by the food industry.”
It is becoming increasingly clear that fat and sugar in combination are capable of producing a dopamine-driven surge of intense pleasure in people with a propensity for addictive behavior. Mice that have been genetic altered so that they lack the ability to taste sweet foods still prefer sugar water to regular water. (See my post on Dopamine and Obesity.) Kessler provides additional evidence that certain forms of overeating qualify as legitimate drug addictions. Just as it is with, say, cocaine addicts, the supersaturated reward pathways of the brain do not have effective mechanisms for signaling: “That’s enough. Stop eating.”
It may seem obvious in retrospect that the same mechanisms that make it so difficult for many drug addicts to “just say no” would also function in the case of addicted overeaters. What happens is similar to the flooding of reward circuitry that occurs in cases of what we might call “compulsive overdrugging,” otherwise known as addiction. The food industry, according to Kessler, has figured out what works, has packaged fat-and-sugar foods in products that scarcely even have to be chewed, and it has priced these products to move.
Yale university conducted studies in which “hypereaters” were given the odor of chocolate during an MRI scan. Normal eaters get used to the odor and habituate rapidly. Hypereaters find that the odor of chocolate becomes more demanding and overpowering with time. And even drinking a complete chocolate milkshake did not quell the craving.
According to Publisher’s Weekly, Kessler’s book, set to be released on April 28, “provides a simple food rehab program to fight back against the [food] industry’s relentless quest for profits while an entire country of people gain weight and get sick.”
Photo Credit: Neurological Correlates
Saturday, 31 January 2009
America Anonymous—Book Review

Sex, drugs, and shoplifting.
New York Times magazine contributor Benoit Denizet-Lewis interweaves eight personal stories of addiction and obsession and ties them in with a well-researched summary of the drug treatment business in his new book, America Anonymous. Offering deft portraits of people suffering from various forms of addiction and compulsion, Denizet-Lewis brings to life much of the denial, prevarication, giddy hopes of victory, incomprehensible relapses, and endless stream of lies and broken promises with which so many active addicts string together their fractured narratives.
By design, Denizet-Lewis swings wide when it comes to defining addiction. In addition to alcoholics and drug addicts, the author, a self-confessed sex addict, includes in his case histories a woman who is a serial shoplifter, a body builder addicted to steroids, a fifty year-old compulsive eater, and a college student addicted to pornography.
“I believe in an expanded understanding of addiction, “ Denizet-Lewis writes. “That is, I believe that gambling, sex, food, spending, and work (to name a few) can, for some people be as addictive and debilitating as an addiction to drugs.”
While I am not as convinced as the author that the scientific evidence is beginning to weigh heavily on the side of accepting behavioral compulsions as classic addictions, I can only agree when he points out that, for all the heady buzz about addiction medicine and pills for alcoholism, 12 Step programs—which originated more than 50 years ago--still arguably represent the most effective approach to treating addiction that we know of. In addition, Denizet-Lewis writes, doctors and clinicians have been promising medical treatments for addiction for 200 years now, and only in the last ten years or so has there been any real progress.
Point taken. The author basically accepts that addictions are chronic diseases with genetic components, “and an onset and course that vary depending on behavior and environmental factors.” Scientific information is presented accurately and in an understandable fashion. Denizet-Lewis knows his subject, even if he uses that data to reach different conclusions than I do. I liked this book, even though I am at odds with many of its arguments.
So, what do Denizet-Lewis’s people teach us about addiction? The crucial need for honesty, to begin with. “If we’re not rigorously honest,” one addict says, “we can’t recover. It’s impossible.” This rule applies to the healers as well. The author quotes one researcher succinctly: “I would distrust anyone who says they can cure addiction.” This sentence alone, if absorbed by addicts seeking treatment, could save them considerable time, money and self-esteem. The author also quotes addiction researcher Anna Rose Childress to good effect: “Relapse is not a failure of treatment. Relapse is part of the disorder.”
What runs through all the personal sagas is the desire of the subjects to feel normal—to “feel feelings” in a normal way. The author offers compelling narratives that catch the flavor of the addicted way of life, a combination of monotony, mood swings, and fear. Denizet-Lewis is particularly adept at making us care about what happens to these people, and we read the book with a hopefulness laced with dread. We know it cannot end happily for everyone. And it does not.
In the end, the author concludes that most forms of addiction can be accounted for by the childhood trauma model. Since a good deal of sex therapy centers on this conception, perhaps the author’s conclusions in this regard are not surprising. However, trauma theories about the origin of addiction have not translated into reliable and effective treatments for addiction, either. And such theories have had a long run, starting even before Freud.
Wednesday, 28 January 2009
"Mood Foods"
Why addicts crave sugar and starch.
James Langton of Clearhead.org.uk recently sent me a fascinating article about food and addiction. The technical bulletin from Sure Screen Diagnostics, Ltd., the U.K.'s leading provider of medical and drug testing services, focuses on the age-old and endlessly fascinating connection between addiction and sugar foods (See my post, “Drug Foods and Addiction”).
Entitled "Mood food and Addiction," the technical bulletin asserts that "drug users, alcoholics and those with addictive tendencies routinely resort to certain psychoactive foods between fixes to regulate their mood." Moreover, "certain foods might reduce withdrawal symptoms... the pantry is a veritable 'psychodelicatessen.'"
While some of the conclusions are highly speculative, most of the article is on more solid ground in its discussion of the "psychopharmacology of everyday foods."
Sweet foods and fruits can mitigate or eliminate cravings, the author says, and examples of this are abundant in the addict and treatment communities. Abstinent cigarette smokers sometimes find that "a piece of fruit or something sweet" can banish cravings by temporarily and partially restoring dopamine and serotonin levels.
In an unconscious effort to raise brain levels of serotonin and dopamine, drug users often discover that doughnuts, cakes, ice cream, soft drinks, and other sugar foods can lessen withdrawal symptoms. As evidence, we are far more likely "to see a user with a bar of chocolate in his hand than a sausage roll."
Complex carbohydrates, the bulletin asserts, do not have the same effect. Whole grain breads and starchy vegetables, unlike table sugar and white bread, do not have the same reinforcing impact on neurotransmitters along the reward pathway. "For that reason, they do not tend to be craved as much as sweets, even though they still satisfy [serotonin] 5-HT needs." Because simple sugars eaten in large quantities can cause blood sugar levels to drop below baseline, the result can be the abrupt return of drug withdrawal symptoms.
How does this work out in practice? The bulletin speculates, for instance, that “a amphetamine user who has exhausted his dopamine and noradrenaline levels, and feels depressed and unable to think straight, may be drawn to high-protein, tyramine-rich foods, such as a steak, pizza or a cheese sandwich and a glass of milk. An MDMA or "ecstasy" user experiencing fatigue... would probably crave something like fish and chips rich in carbohydrates, and a sugar-rich drink to temporarily bring the depleted 5-HT levels back up to normal." As for opiate users, foods such as whole milk, ice cream, and milk chocolate are appealing because they contain "biologically active opioid peptides.... It no doubt explains why a pint of full fat milk and a Snicker's bar is a perennial snacking favourite of opiate users."
As for chocolate (you didn’t think I’d forget chocolate, did you?), “the most widely preferred chocolate among the general population is not unsweetened dark chocolate with its higher drug cocktail, but sweetened milk chocolate suggesting that the majority of us may in fact be craving its addictive psychoactive sugars, fats and narcotic casomorphins more than anything else.”
In the end, the specific food preferences of addicts force us “to reconsider how fragile the food-drug distinction actually is.”
Graphic Credit: Anselm
Sunday, 28 December 2008
[Guest Post] Food For Thought--Are You Addicted?

Can you eat your way to happiness?
(This article is contributed by Sarah Scrafford, who regularly writes on the topic of Becoming an Ultrasound Technician. She invites your questions, comments and freelancing job inquiries at her email address: sarah.scrafford25@gmail.com.)
Food is essential for life, but there are times when it becomes the reason for death. If you’ve heard of addictions, you’ll know what I’m talking about – addictions and substance dependence extend beyond the realm of drugs, nicotine and alcohol. There are times when it can become as simple, and as complicated, as being addicted to food. Some people have a sweet tooth and get their rush from sugar; others limit themselves to chocolate; but there are a few people who need to eat all the time – they eat when they’re sad and when they’re happy; they eat because food is available; they eat because they’re bored; they eat because they’re stressed; in short, they eat all possible reasons and for no reason at all.
Too much of anything is bad for you, and so you have food and eating related disorders. The compulsive eaters are beset with various medical problems, all of which begin and end with obesity. Large people with fat deposits on various parts of their body are prone to illnesses like diabetes, hypertension, stroke and cardiac diseases. They’re also bound to be in poor general health because of their low level of fitness and sedentary lifestyle that comes about automatically when you’re fat and unable to move around without difficulty. Besides these, they’re also plagued by knee and back pains because of their weight – their knees are unable to support their body weight and become weak as time goes by.
On the other end of the spectrum are those obsessed with thinness – they love to eat too, but they do it on the sly. And when they’re done, they make themselves throw up either by retching or by using emetics. This disease, called bulimia, is characteristic of food addicts who feel guilty that they eat so much, and who are scared of the weight they’re going to put on because of the amount they’ve consumed. Bulimics are prone to binge eating, where they eat much more than normal amounts.
The best cure to an eating disorder or food addiction is self-control, and if you cannot control yourself, then get someone to help you do so. De-addiction from alcohol, tobacco or any other drug happens when you avoid the substance altogether, but it’s not that easy to overcome an addiction to something that’s a basic necessity for life. The trick is to learn to count your calories or to get someone to do it for you. You could also begin a sensible exercise routine where you concentrate on losing weigh in a healthy manner. A more active lifestyle gives you less time to sit around doing nothing, and so frequenting the path between your couch and your refrigerator.
Food addiction, like all other addictions, is a psychological problem that can be cured if treated at an early stage. All you need is a lot of will power and a little determination.
Subscribe to:
Posts (Atom)

